Will Calcaneal Apophysitis Often Require Surgical Treatments?
What is sever's disease? sever's disease is a common cause of heel pain in active children. Sever's disease, also called calcaneal apophysitis, occurs when the growth plate of the heel is injured by excessive forces during early adolescence.
Causes
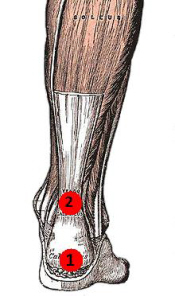
During the growth spurt of early puberty, the heel bone (also called the calcaneus) sometimes grows faster than the leg muscles and tendons. This can cause the muscles and tendons to become very tight and overstretched, making the heel less flexible and putting pressure on the growth plate. The Achilles tendon (also called the heel cord) is the strongest tendon that attaches to the growth plate in the heel. Over time, repeated stress (force or pressure) on the already tight Achilles tendon damages the growth plate, causing the swelling, tenderness, and pain of Sever's disease. Such stress commonly results from physical activities and sports that involve running and jumping, especially those that take place on hard surfaces, such as track, basketball, soccer, and gymnastics.
Symptoms
Acute pain, pain asscoiatied with Sever?s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running. Highly active - children who are very active are among the most susceptible in experiencing Sever?s disease, because of the stress and tension placed on their feet.
Diagnosis
You may have pain when your doctor squeezes your heel bone. You may have pain when asked to stand or walk on your toes or on your heels. You may have pain in your heel when your doctor stretches your calf muscles. Your doctor may order x-rays of the injured foot to show an active growth plate.
Non Surgical Treatment
Reduce inflammation:
Ice: For at least 20 minutes after activity or when pain increases.
Nonsteroidal anti-inflammatory drugs:(NSAIDs) may also help. Stretch the calf. Increase calf flexibility by doing calf stretches for 30 to 45 seconds several times per day.
Protect the heel: The shoe may need to be modified to provide the proper heel lift or arch support.
Select a shoe with good arch support and heel lift if possible. Try heel lifts or heel cups in sports shoes, especially cleats. Try arch support in cleats if flat feet contribute to the problem.
Take it one step at a time:. Gradually resume running and impact activities as symptoms allow. Sever?s disease usually goes away when the growth plate (apophysis) matures, which should be by age 12 to 13 years in females and 13 to 14 years in males.
Surgical Treatment
The surgeon may select one or more of the following options to treat calcaneal apophysitis. Reduce activity. The child needs to reduce or stop any activity that causes pain. Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue. Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile. Often heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis, or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.
Acquired Flat Foot Tibialis Posterior Tenosynovitis
Overview
The posterior tibial tendon serves as one of the major supporting structures of the foot, helping it to function while walking. Posterior tibial tendon dysfunction (PTTD) is a condition caused by changes in the tendon, impairing its ability to support the arch. This results in flattening of the foot. PTTD is often called ?adult acquired flatfoot? because it is the most common type of flatfoot developed during adulthood. Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse, especially if it isn?t treated early. 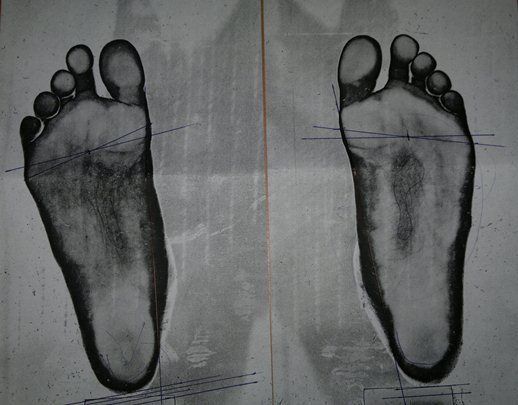
Causes
As discussed above, many different problems can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to support the arch of your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Inflammatory arthritis, such as rheumatoid arthritis, can cause a painful flatfoot. This type of arthritis attacks not only the cartilage in the joints, but also the ligaments that support the foot. Inflammatory arthritis not only causes pain, but also causes the foot to change shape and become flat. The arthritis can affect the back of the foot or the middle of foot, both of which can result in a fallen arch. An injury to the tendons or ligaments in the foot can cause the joints to fall out of alignment. The ligaments support the bones and prevent them from moving. If the ligaments are torn, the foot will become flat and painful. This more commonly occurs in the middle of the foot (Lisfranc injury), but can also occur in the back of the foot. Injuries to tendons of the foot can occur either in one instance (traumatically) or with repeated use over time (overuse injury). Regardless of the cause, if tendon function is altered, the forces that are transmitted across joints in the foot are changed and this can lead to increased stress on joint cartilage and ligaments. In addition to tendon and ligament injuries, fractures and dislocations of the bones in the midfoot can also lead to a flatfoot deformity. People with diabetes or with nerve problems that limits normal feeling in the feet, can have collapse of the arch or of the entire foot. This type of arch collapse is typically more severe than that seen in patients with normal feeling in their feet. In addition to the ligaments not holding the bones in place, the bones themselves can sometimes fracture and disintegrate without the patient feeling any pain. This may result in a severely deformed foot that is very challenging to correct with surgery. Special shoes or braces are the best method for dealing with this problem.
Symptoms
Many patients with this condition have no pain or symptoms. When problems do arise, the good news is that acquired flatfoot treatment is often very effective. Initially, it will be important to rest and avoid activities that worsen the pain.
Diagnosis
In the early stages of dysfunction of the posterior tibial tendon, most of the discomfort is located medially along the course of the tendon and the patient reports fatigue and aching on the plantar-medial aspect of the foot and ankle. Swelling is common if the dysfunction is associated with tenosynovitis. As dysfunction of the tendon progresses, maximum pain occurs laterally in the sinus tarsi because of impingement of the fibula against the calcaneus. With increasing deformity, patients report that the shape of the foot changes and that it becomes increasingly difficult to wear shoes. Many patients no longer report pain in the medial part of the foot and ankle after a complete rupture of the posterior tibial tendon has occurred; instead, the pain is located laterally. If a fixed deformity has not occurred, the patient may report that standing or walking with the hindfoot slightly inverted alleviates the lateral impingement and relieves the pain in the lateral part of the foot.
Non surgical Treatment
Non-surgical treatment includes rest and reducing your activity until the pain improves. Orthotics or bracing help support the tendon to reduce its pull along the arch, thus reducing pain. In moderate to severe cases, a below knee cast or walking boot may be needed to allow the tendon to rest completely and heal. Physical therapy is an integral part of the non-surgical treatment regimen to reduce inflammation and pain. Anti-inflammatory medication is often used as well. Many times evaluation of your current shoes is necessary to ensure you are wearing appropriate shoe gear to prevent re-injury. 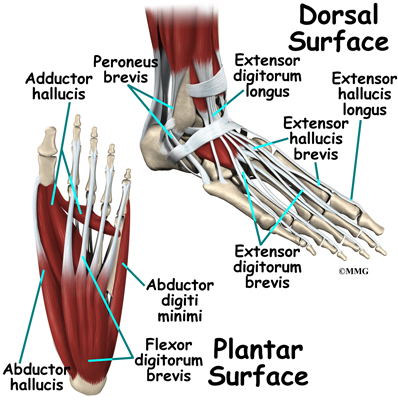
Surgical Treatment
Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
What Is The Treatment And Cause For Adult Aquired FlatFoot
One in four adults in the U.S. has adult acquired flatfoot deformity, which may begin during childhood or be acquired with age. The foot may be flat all the time or may lose its arch when the person stands. The most common and serious cause of flat foot is Posterior Tibial Tendon Dysfunction, in which the main tendon that supports the arch gradually weakens.

Causes
There are numerous causes of acquired Adult Flatfoot, including, trauma, fracture, dislocation, tendon rupture/partial rupture or inflammation of the tendons, tarsal coalition, arthritis, neuroarthropathy and neurologic weakness. The most common cause of acquired Adult Flatfoot is due to overuse of a tendon on the inside of the ankle called the posterior tibial tendon. This is classed as - posterior tibial tendon dysfunction. What are the causes of Adult Acquired flat foot? Trauma, Fracture or dislocation. Tendon rupture, partial tear or inflammation. Tarsal Coalition. Arthritis. Neuroarthropathy. Neurological weakness.
Symptoms
Often, this condition is only present in one foot, but it can affect both. Adult acquired flatfoot symptoms vary, but can swelling of the foot's inner side and aching heel and arch pain. Some patients experience no pain, but others may experience severe pain. Symptoms may increase during long periods of standing, resulting in fatigue. Symptoms may change over time as the condition worsens. The pain may move to the foot's outer side, and some patients may develop arthritis in the ankle and foot.
Diagnosis
There are four stages of adult-acquired flatfoot deformity (AAFD). The severity of the deformity determines your stage. For example, Stage I means there is a flatfoot position but without deformity. Pain and swelling from tendinitis is common in this stage. Stage II there is a change in the foot alignment. This means a deformity is starting to develop. The physician can still move the bones back into place manually (passively). Stage III adult-acquired flatfoot deformity (AAFD) tells us there is a fixed deformity. This means the ankle is stiff or rigid and doesn???t move beyond a neutral (midline) position. Stage IV is characterized by deformity in the foot and the ankle. The deformity may be flexible or fixed. The joints often show signs of degenerative joint disease (arthritis).
Non surgical Treatment
Medical or nonoperative therapy for posterior tibial tendon dysfunction involves rest, immobilization, nonsteroidal anti-inflammatory medication, physical therapy, orthotics, and bracing. This treatment is especially attractive for patients who are elderly, who place low demands on the tendon, and who may have underlying medical problems that preclude operative intervention. During stage 1 posterior tibial tendon dysfunction, pain, rather than deformity, predominates. Cast immobilization is indicated for acute tenosynovitis of the posterior tibial tendon or for patients whose main presenting feature is chronic pain along the tendon sheath. A well-molded short leg walking cast or removable cast boot should be used for 6-8 weeks. Weight bearing is permitted if the patient is able to ambulate without pain. If improvement is noted, the patient then may be placed in custom full-length semirigid orthotics. The patient may then be referred to physical therapy for stretching of the Achilles tendon and strengthening of the posterior tibial tendon. Steroid injection into the posterior tibial tendon sheath is not recommended due to the possibility of causing a tendon rupture. In stage 2 dysfunction, a painful flexible deformity develops, and more control of hindfoot motion is required. In these cases, a rigid University of California at Berkley (UCBL) orthosis or short articulated ankle-foot orthosis (AFO) is indicated. Once a rigid flatfoot deformity develops, as in stage 3 or 4, bracing is extended above the ankle with a molded AFO, double upright brace, or patellar-tendon-bearing brace. The goals of this treatment are to accommodate the deformity, prevent or slow further collapse, and improve walking ability by transferring load to the proximal leg away from the collapsed medial midfoot and heel.

Surgical Treatment
If conservative treatment fails to provide relief of pain and disability then surgery is considered. Numerous factors determine whether a patient is a surgical candidate. They include age, obesity, diabetes, vascular status, and the ability to be compliant with post-operative care. Surgery usually requires a prolonged period of nonweightbearing immobilization. Total recovery ranges from 3 months to one year. Clinical, x-ray, and MRI examination are all used to select the appropriate surgical procedure.
Achilles Tendonitis Treatment And Cause
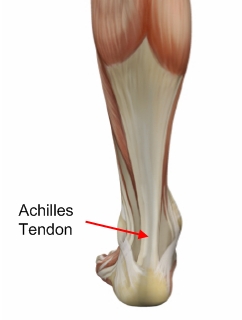 Achilles tendinitis is an overuse injury of the Achilles tendon, the band of tissue that connects calf muscles at the back of the lower leg to your heel bone. Achilles tendinitis most commonly occurs in runners who have suddenly increased the intensity or duration of their runs. It's also common in middle-aged people who play sports, such as tennis or basketball, only on the weekends. Most cases of Achilles tendinitis can be treated with relatively simple, at-home care under your doctor's supervision. Self-care strategies are usually necessary to prevent recurring episodes. More-serious cases of Achilles tendinitis can lead to tendon tears (ruptures) that may require surgical repair.
Achilles tendinitis is an overuse injury of the Achilles tendon, the band of tissue that connects calf muscles at the back of the lower leg to your heel bone. Achilles tendinitis most commonly occurs in runners who have suddenly increased the intensity or duration of their runs. It's also common in middle-aged people who play sports, such as tennis or basketball, only on the weekends. Most cases of Achilles tendinitis can be treated with relatively simple, at-home care under your doctor's supervision. Self-care strategies are usually necessary to prevent recurring episodes. More-serious cases of Achilles tendinitis can lead to tendon tears (ruptures) that may require surgical repair.
Causes
As ?overuse? disorders, Achilles tendonitis and tendonosis are usually caused by a sudden increase of a repetitive activity involving the Achilles tendon. Such activity puts too much stress on the tendon too quickly, leading to micro-injury of the tendon fibers. Due to this ongoing stress on the tendon, the body is unable to repair the injured tissue. The structure of the tendon is then altered, resulting in continued pain. Achilles4Athletes are at high risk for developing disorders of the Achilles tendon. Achilles tendonitis and tendonosis are also common in individuals whose work puts stress on their ankles and feet, such as laborers, as well as in ?weekend warriors?-those who are less conditioned and participate in athletics only on weekends or infrequently. In addition, people with excessive pronation (flattening of the arch) have a tendency to develop Achilles tendonitis and tendonosis due to the greater demands placed on the tendon when walking. If these individuals wear shoes without adequate stability, their over-pronation could further aggravate the Achilles tendon.
Symptoms
Recurring localized pain, sometimes severe, along the tendon during or a few hours after running. Morning tenderness about an inch and a half above the point where the Achilles tendon is attached to the heel bone. Sluggishness in your leg. Mild or severe swelling. Stiffness that generally diminishes as the tendon warms up with use.
Diagnosis
Examination of the achilles tendon is inspection for muscle atrophy, swelling, asymmetry, joint effusions and erythema. Atrophy is an important clue to the duration of the tendinopathy and it is often present with chronic conditions. Swelling, asymmetry and erythema in pathologic tendons are often observed in the examination. Joint effusions are uncommon with tendinopathy and suggest the possibility of intra-articular pathology. Range of motion testing, strength and flexibility are often limited on the side of the tendinopathy. Palpation tends to elicit well-localized tenderness that is similar in quality and location to the pain experienced during activity. Physical examinations of the Achilles tendon often reveals palpable nodules and thickening. Anatomic deformities, such as forefoot and heel varus and excessive pes planus or foot pronation, should receive special attention. These anatomic deformities are often associated with this problem. In case extra research is wanted, an echography is the first choice of examination when there is a suspicion of tendinosis. Imaging studies are not necessary to diagnose achilles tendonitis, but may be useful with differential diagnosis. Ultrasound is the imaging modality of first choice as it provides a clear indication of tendon width, changes of water content within the tendon and collagen integrity, as well as bursal swelling. MRI may be indicated if diagnosis is unclear or symptoms are atypical. MRI may show increased signal within the Achilles.
Nonsurgical Treatment
Make sure that the tendon is not torn through and through. If it is severed, you must see a doctor immediately so that the tendon can be repaired. Severe injuries can sever a tendon, without a skin laceration being present. Testing involves moving the toes and foot to see if the tendon moves. If the tendon does not appear to move, it may be severed (comparing the injured tendon and its movement to the same tendon on the uninjured foot may help). Very sharp pain, a sudden pop, or an obvious gap in the structure of the tendon are all signs of a rupture, and should be seen by a doctor as soon as possible. If there is extreme swelling of the leg, and pain (out of proportion to the amount of trauma received), you may have sustained a vascular injury. A doctor must see this type of injury immediately. If you are not sure, see a doctor. If you have multiple injured areas see a doctor immediately, in order to prevent excessive swelling and pain. If the above exam is negative, then you may proceed with self-treatment. (However, if you are not sure of the extent of your injury, you should consult your doctor immediately). The sooner you begin to treat your injury by following "R.I.C.E.", the better you will feel. Rest is very important. Take off your shoe, get off your feet, and relax. Ice should be applied as soon as possible. Never apply ice directly on the injured area, as the cold may make the pain worse. Ice should be applied close to the injured site, between the heart and the injury, so that as the blood flows under the ice, it will be cooled. This cool blood flowing into the injured area will help to reduce the swelling and pain. Apply the ice, wrapped in a cloth or over an elastic bandage, to the foot for 15 minutes, every 1-2 hours, for up to 3 days after an injury. If the ice is uncomfortable, or causes increased pain, do not continue to use it, and see a doctor. If you have poor circulation do not use ice, as this may cause a serious problem. c. Compression is used to limit swelling, and to give support to the injured area. Compression should be applied to the entire foot, starting first at the toes and working back to the ankle. If it is applied just to the injured area, increased swelling will occur in front and behind the wrapping. Compression should be applied with a 3-inch elastic bandage, beginning around the base of all the toes, and then going around the foot and ankle. Continue over the calf muscle when possible. Compression reduces motion in the injured area and foot, and this decreases the pain, and allows for quicker healing. The bandage should not be so tight that it causes increased pain or throbbing in the toes or foot. It should be comfortable! Do not remove the elastic bandage for the first 12 hours, unless it becomes too tight, or the pain increases, or the toes become pale, blue, or cool. If any of these things happen, immediately remove all bandages, and leave them off for several hours. The normal color and temperature of the toes should return immediately. If not, see a doctor immediately! Continue until the swelling and pain subsides; it could take from several days to several weeks. d. Elevation of the leg will aid in reducing swelling and pain. Blood rushes to an injured area to bring increased blood cells, that aid in healing. Gravity will also force blood to the injured area. Too many cells and too much fluid will apply pressure to the injured nerves and tissues, and cause increased pain and delayed healing. Keep your foot elevated so that it is at least parallel to the ground, or higher if it is comfortable. Do this for at least 48 hours, or until the throbbing subsides, when you lower the leg.
Surgical Treatment
Histological and biological studies on tendon healing have made it possible to envisage surgical repair using a percutaneous approach, with the following objectives, a minimal, and not very aggressive, operation, which is quick and easy and within the capabilities of all surgeons, the shortest hospitalisation period possible, above all, early and effective re-education, providing a satisfactory result both in terms of solidity and the comfort of the patient. The percutaneous tenosynthesis TENOLIG combines stability, reliability, patient comfort and lower overall social and professional costs for this type of lesion.
Prevention
Do strengthening and stretching exercises to keep calf muscles strong and flexible. Keep your hamstring muscles flexible by stretching. Warm up and stretch adequately before participating in any sports. Always increase the intensity and duration of training gradually. Do not continue an exercise if you experience pain over the tendon. Wear properly fitted running and other sports shoes, including properly fitted arch supports if your feet roll inwards excessively (over-pronate).
What Exactly Can Cause Heel Discomfort

Overview
Plantar Fasciitis is the Latin term for "inflammation of the plantar fascia". The plantar fascia is a thick, fibrous ligament that runs under the foot from the heel bone to the toes. It forms the arch of the foot and functions as our natural shock-absorbing mechanism. Unlike muscle tissue, the plantar fascia is not very elastic and therefore is very limited in its capacity to stretch or elongate. Herein lies the problem, when too much traction is placed on the plantar fascia (for various reasons) micro-tearing will occur, resulting in irritation, inflammation and pain. Plantar Fasciitis usually causes pain under the heel. However some people may experience pain under the arch of the foot. Both heel pain and arch discomfort are related to Plantar Fasciitis, with heel pain being far more common than arch pain.
Causes
Far and away the most common cause of plantar fasciitis in an athlete is faulty biomechanics of the foot or leg. Faulty biomechanics causes the foot to sustain increased or prolonged stresses over and above those of routine ground contacts. Throughout the phase of ground contact, the foot assumes several mechanical positions to dissipate shock while at the same time placing the foot in the best position to deliver ground forces. With heel landing the foot is supinated (ankle rolled out). At mid-stance the foot is pronated (ankle rolled in). The foot is supinated again with toe-off. The supination of the foot at heel strike and toe-off makes the foot a rigid lever. At heel strike the shock of ground contact is transferred to the powerful quads. During toe-off forward motion is created by contraction of the gastroc complex plantar flexing the rigid lever of the foot pushing the body forward.
Symptoms
The symptoms of plantar fasciitis include pain in the bottom of your foot, especially at the front or centre of the heel bone, pain that is worse when first rising in the morning (called "first-step pain"), when first standing up after any long period of sitting, or after increased levels of activity especially in non-supportive shoes. Seek medical advice about plantar fasciitis if you have heel pain or pain in the bottom of your foot, especially when you get up in the morning, that does not respond to treatment or if there is redness or bruising in the heel.
Diagnosis
Your doctor will perform a physical exam to check for tenderness in your foot and the exact location of the pain to make sure that it’s not caused by a different foot problem. The doctor may ask you to flex your foot while he or she pushes on the plantar fascia to see if the pain gets worse as you flex and better as you point your toe. Mild redness or swelling will also be noted. Your doctor will evaluate the strength of your muscles and the health of your nerves by checking your reflexes, your muscle tone, your sense of touch and sight, your coordination, and your balance. X-rays or a magnetic resonance imaging (MRI) scan may be ordered to check that nothing else is causing your heel pain, such as a bone fracture.
Non Surgical Treatment
Over-the-counter arch supports may be useful in patients with acute plantar fasciitis and mild pes planus. The support provided by over-the-counter arch supports is highly variable and depends on the material used to make the support. In general, patients should try to find the most dense material that is soft enough to be comfortable to walk on. Over-the-counter arch supports are especially useful in the treatment of adolescents whose rapid foot growth may require a new pair of arch supports once or more per season. Custom orthotics are usually made by taking a plaster cast or an impression of the individual's foot and then constructing an insert specifically designed to control biomechanical risk factors such as pes planus, valgus heel alignment and discrepancies in leg length. For patients with plantar fasciitis, the most common prescription is for semi-rigid, three-quarters to full-length orthotics with longitudinal arch support. Two important characteristics for successful treatment of plantar fasciitis with orthotics are the need to control over-pronation and metatarsal head motion, especially of the first metatarsal head. In one study, orthotics were cited by 27 percent of patients as the best treatment. The main disadvantage of orthotics is the cost, which may range from $75 to $300 or more and which is frequently not covered by health insurance.

Surgical Treatment
In cases that do not respond to any conservative treatment, surgical release of the plantar fascia may be considered. Plantar fasciotomy may be performed using open, endoscopic or radiofrequency lesioning techniques. Overall, the success rate of surgical release is 70 to 90 percent in patients with plantar fasciitis. Potential risk factors include flattening of the longitudinal arch and heel hypoesthesia as well as the potential complications associated with rupture of the plantar fascia and complications related to anesthesia.
Stretching Exercises
The following exercises are commonly prescribed to patients with this condition. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 2 - 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate and advanced exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head until you feel a stretch in the back of your calf, Achilles tendon, plantar fascia or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free. Resistance Band Calf Strengthening. Begin this exercise with a resistance band around your foot as demonstrated and your foot and ankle held up towards your head. Slowly move your foot and ankle down against the resistance band as far as possible and comfortable without pain, tightening your calf muscle. Very slowly return back to the starting position. Repeat 10 - 20 times provided the exercise is pain free.
What Is Heel Discomfort

Overview
Foot pain affects nearly all people at one time or another. It can also lead to other musculoskeletal problems such as ankle, knee and back pain (Hill et al., 2008). This pain negatively affects one’s quality of life and ability to enjoy workouts and/or maintain a regular program of exercise. One of the most common sources of foot pain is plantar fasciitis, a condition where the connective tissue on the underside of the foot becomes irritated and painful as a result of an injury, overuse or misuse. The plantar fascia is a system of connective tissue that runs from your heel to just behind your toes. During weightbearing activities, such as walking or running, your body weight is transferred onto your foot from your heel to your toes (which results in your toes moving away from your heel). This spreading out of the foot places tension on the plantar fascia because it connects those two parts. If the tension on this structure is too great or is not dispersed evenly, the plantar fascia can develop microtears and become irritated and painful, resulting in a condition called plantar fasciitis.
Causes
Plantar Fasciitis is caused by abnormal pronation of the foot. Contributing factors are obesity, weight gain, jobs that require a lot of walking or standing on hard surfaces, badly worn shoes with little support, and also inactivity. As a result of over-pronation, with every step the Plantar Fascia (band of tissue under the foot) is being stretched, resulting in inflammation, irritation and pain at the attachment of the fascia into the heel bone. In some cases the pain is felt under the foot, in the arch. Continuous pulling of the fascia at the heel bone, eventually may lead to the development of bony growth on the heel. This is called a heel spur. When you’re at rest, such as while sleeping, the Plantar Fascia tightens and shortens. When body weight is rapidly applied to the foot, the Fascia must stretch and quickly lengthen, causing micro-tears in the Fascia. As a result, the foot pain is more severe with your first steps in the morning, or after sitting for a long period. Plantar Fasciitis is more likely to happen if you suffer from over-pronation (flattening of the arch), you stand or walk on hard surfaces, for long periods, you are overweight or pregnant, you have tight calf muscles.
Symptoms
The major complaint of those with plantar fasciitis is pain and stiffness in the bottom of the heel. This develops gradually over time. It usually affects just one foot, but can affect both feet. Some people describe the pain as dull, while others experience a sharp pain, and some feel a burning or ache on the bottom of the foot extending outward from the heel. The pain is usually worse in the morning when you take your first steps out of bed, or if you’ve been sitting or lying down for a while. Climbing stairs can be very difficult due to the heel stiffness. After prolonged activity, the pain can flare-up due to increased inflammation. Pain is not usually felt during the activity, but rather just after stopping.
Diagnosis
Your doctor will check your feet and watch you stand and walk. He or she will also ask questions about your past health, including what illnesses or injuries you have had. Your symptoms, such as where the pain is and what time of day your foot hurts most. How active you are and what types of physical activity you do. Your doctor may take an X-ray of your foot if he or she suspects a problem with the bones of your foot, such as a stress fracture.
Non Surgical Treatment
Biomechanical plantar fasciitis can be easily reduced by correcting misalignment of the feet. Wearing orthopedic shoes for plantar fasciitis and orthotic inserts is an easy, effective method of naturally realigning the foot. Worn consistently from first thing in the morning to last thing at night, orthotic support can reduce and sometimes eliminate plantar fasciitis. Biomechanical plantar fasciitis can be easily reduced by correcting misalignment of the feet. Wearing orthopedic shoes for plantar fasciitis and orthotic inserts is an easy, effective method of naturally realigning the foot. Worn consistently from first thing in the morning to last thing at night, orthotic support can reduce and sometimes eliminate plantar fasciitis. Preserve Your Arch with Strengthening Exercises. While seated and barefoot, squeeze your foot as if you have a small marble under the ball of your foot. If you just happen to have a few marbles handy, you can actually practice picking them up between your toes and ball of your foot - and then set them down again. This stretches and helps strengthen the muscles that run under metatarsals (the longest bones in the foot which create its arched shape). Slowly Increase Physical Activity. If you're a runner, a tried and true method of preventing over-use injuries is to only increase your mileage by 10% weekly, max. If you’re new to a walking program, the same caution should be exercised. Ice and Rest. After mild stretching, use a frozen water bottle to roll under the arch of your foot for 10-20 minutes. It may be possible to make an active recovery by wearing Orthaheel Technology to keep your feet naturally aligned, therefore reducing strain on the plantar fascia, while moving throughout your day.

Surgical Treatment
Most practitioners agree that treatment for plantar fasciitis is a slow process. Most cases resolve within a year. If these more conservative measures don't provide relief after this time, your doctor may suggest other treatment. In such cases, or if your heel pain is truly debilitating and interfering with normal activity, your doctor may discuss surgical options with you. The most common surgery for plantar fasciitis is called a plantar fascia release and involves releasing a portion of the plantar fascia from the heel bone. A plantar fascia release can be performed through a regular incision or as endoscopic surgery, where a tiny incision allows a miniature scope to be inserted and surgery to be performed. About one in 20 patients with plantar fasciitis will need surgery. As with any surgery, there is still some chance that you will continue to have pain afterwards.
Prevention
Preventing plantar fasciitis is crucial. There are many choices to help prevent the occurrence of this condition, and keep it from returning. One of the most important is maintaining a healthy weight in order to reduce tension on the plantar fascia. In addition, shoes are very important, and should fit well and provide ample cushioning and support throughout the heel, arch, and ball of the foot so that weight is distributed evenly throughout the foot. Try to avoid walking barefoot on hard surfaces and replace old shoes before they wear out, especially shoes that you run or exercise in. When exercising, start off slow and ease into new routines to prevent sudden or excessive stress on tissue. Lastly, keep your calf muscles and the tissue of your feet stretched. Greater flexibility in the tissue makes them less susceptible to damage.
What Causes Heel Discomfort To Flare Up

Overview
Plantar fasciitis is a common foot disorder that affects more than two million people every year, especially runners. It is inflammation of the plantar fascia, a thick band of tissue on the bottom of the foot. The most common area of pain is directly on the bottom of the heel, although some people may only have pain in the arch of the foot. Diagnosis of plantar fasciitis is typically done through a physical examination, which includes listening to the patient history, palpation of the heel and possibly x-rays.
Causes
Plantar fasciitis is caused by small, repetitive trauma to the plantar fascia. This trauma can be due to activity that puts extra stress on the foot. Plantar fasciitis is most common in people who are 40-60 years old. Other risk factors that increase your chance of getting plantar fasciitis include physical exertion, especially in sports such as running, Volleyball, tennis, a sudden increase in exercise intensity or duration, physical activity that stresses the plantar fascia. People who spend a lot of time standing, a sudden increase in activities that affect the feet, obesity or weight gain, pre-existing foot problems, including an abnormally tight Achilles tendon, flat feet, or an ankle that rolls inward too much. Poor footwear. Heel spurs.
Symptoms
The main symptom of plantar fasciitis is heel pain when you walk. You may also feel pain when you stand and possibly even when you are resting. This pain typically occurs first thing in the morning after you get out of bed, when your foot is placed flat on the floor. The pain occurs because you are stretching the plantar fascia. The pain usually lessens with more walking, but you may have it again after periods of rest. You may feel no pain when you are sleeping because the position of your feet during rest allows the fascia to shorten and relax.
Diagnosis
Your GP or podiatrist (a healthcare professional who specialises in foot care) may be able to diagnose the cause of your heel pain by asking about your symptoms and examining your heel and foot. You will usually only need further tests if you have additional symptoms that suggest the cause of your heel pain is not inflammation, such as numbness or a tingling sensation in your foot, this could be a sign of nerve damage in your feet and legs (peripheral neuropathy) your foot feels hot and you have a high temperature (fever) of 38C (100.4F) or above - these could be signs of a bone infection, you have stiffness and swelling in your heel, this could be a sign of arthritis. Possible further tests may include blood tests, X-rays - where small doses of radiation are used to detect problems with your bones and tissues, a magnetic resonance imaging (MRI) scan or ultrasound scan, which are more detailed scans.
Non Surgical Treatment
Plantar fasciitis can be a difficult problem to treat, with no panacea available. Fortunately, most patients with this condition eventually have satisfactory outcomes with nonsurgical treatment. Therefore, management of patient expectations minimizes frustration for both the patient and the provider.

Surgical Treatment
The most dramatic therapy, used only in cases where pain is very severe, is surgery. The plantar fascia can be partially detached from the heel bone, but the arch of the foot is weakened and full function may be lost. Another surgery involves lengthening the calf muscle, a process called gastrocnemius recession. If you ignore the condition, you can develop chronic heel pain. This can change the way you walk and cause injury to your legs, knees, hips and back. Steroid injections and some other treatments can weaken the plantar fascia ligament and cause potential rupture of the ligament. Surgery carries the risks of bleeding, infection, and reactions to anesthesia. Plantar fascia detachment can also cause changes in your foot and nerve damage. Gastrocnemius resection can also cause nerve damage.
Prevention
It is not always possible to prevent heel pain, but there are measures you can take to help avoid further episodes. Healthy weight. Being overweight can place excess pressure and strain on your feet, particularly on your heels. This increases the risk of damaging your feet and heels. If you are overweight, losing weight and maintaining a healthy weight by combining regular exercise with a healthy, balanced diet can be beneficial for your feet. You can calculate your body mass index (BMI) to find out whether you are a healthy weight for your height and build. To work out your BMI, divide your weight in kilograms by your height in metres squared. A BMI of less than 18.5 means that you are underweight, 18.5-24.9 means that your weight is healthy, 25-29 means that you are overweight, 30-40 means that you are obese, over 40 means that you are morbidly obese. You can also use the BMI healthy weight calculator to work out your BMI. Healthy feet. You should always wear footwear that is appropriate for your environment and day-to-day activities. Wearing high heels when you go out in the evening is unlikely to be harmful. However, wearing them all week at work may damage your feet, particularly if your job involves a lot of walking or standing. Ideally, you should wear shoes with laces and a low to moderate heel that supports and cushions your arches and heels. Avoid wearing shoes with no heels.