Bursitis Ball Of Foot Care
There are many reasons for pain in your heel, but one common pain is heel bursitis. This condition makes simple tasks like walking around your home painful. Understand the causes, symptoms and treatments of bursitis of the heel, and determine if it is causing your heel pain.
Causes
Your ankle bursitis may have been caused by one or more of the following Pressure on your ankle and heels. This is often caused by running or exercising on uneven ground. The way that you exercise may also cause ankle bursitis or make it worse. It may be caused by wearing poorly fitting shoes that constantly rub against the heel. Direct, hard hit to your heel. Infection (in-FEK-shun). Medical problems such as rheumatoid (ROO-ma-toid) arthritis (ahr-THREYE-tis) or gout. Overusing your ankles. This is caused by doing activities or sports that use the same motions (movements) over and over again. Examples of repeating motions are running, walking, or jumping. Sometimes people do not know how they developed ankle bursitis.
Symptoms
Posterior heel pain is the chief complaint in individuals with calcaneal bursitis. Patients may report limping caused by the posterior heel pain. Some individuals may also report an obvious swelling (eg, a pump bump, a term that presumably comes from the swelling's association with high-heeled shoes or pumps). The condition may be unilateral or bilateral. Symptoms are often worse when the patient first begins an activity after rest.
Diagnosis
Careful examination by your physician or physiotherapist can determine if the inflammation is from the Achilles tendon or from the retrocalcaneal bursa. Tenderness due to insertional Achilles tendinitis is normally located slightly more distal where the tendon inserts into the back of the heel, whereas tenderness caused by the retrocalcaneal bursa is normally palpable at the sides of the distal Achilles tendon. Diagnosis can be confirmed with an ultrasound investigation, MRI or CT scan.
Non Surgical Treatment
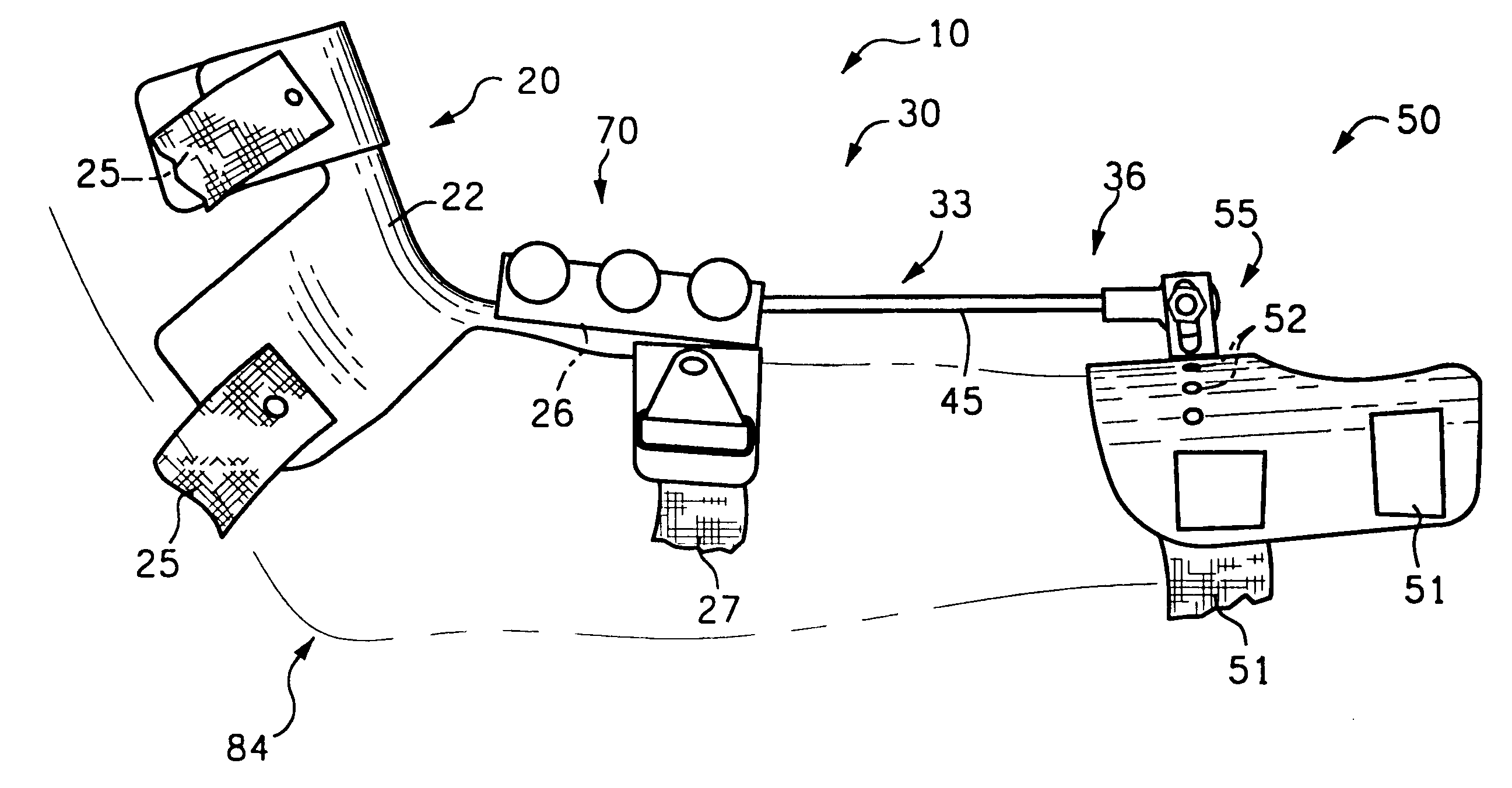
There are a variety of treatments for bursitis of the heel. Bursitis on the bottom of your heel (which is called infracalcaneal bursitis) is common in heels with thinning fat pads. Gel heel cushions or custom made orthotics (that have a horse-shoe cut and extra foam in the heel) can be lifesavers in reducing the pain. For bursitis of the posterior heel (retrocalcaneal bursitis), try to avoid going barefoot and to reduce the stress on the Achilles tendon by not over flexing your heel, the tighter your Achilles becomes, the more you compress the bursa sacs of the posterior heel. Heel lifts can help this, or wearing shoes with elevated heels (note that this method is not sanctioning high heels, as high heels can provide little comfort or support and usually are tight in the areas where your bursitis is most inflamed). Products such as AirHeel made by Aircast can help massage the bottom and back of the heel, helping to decrease pain.
Surgical Treatment
Surgery. Though rare, particularly challenging cases of retrocalcaneal bursitis might warrant a bursectomy, in which the troublesome bursa is removed from the back of the ankle. Surgery can be effective, but operating on this boney area can cause complications, such as trouble with skin healing at the incision site. In addition to removing the bursa, a doctor may use the surgery to treat another condition associated with the retrocalcaneal bursitis. For example, a surgeon may remove a sliver of bone from the back of the heel to alter foot mechanics and reduce future friction. Any bone spurs located where the Achilles attaches to the heel may also be removed. Regardless of the conservative treatment that is provided, it is important to wait until all pain and swelling around the back of the heel is gone before resuming activities. This may take several weeks. Once symptoms are gone, a patient may make a gradual return to his or her activity level before their bursitis symptoms began. Returning to activities that cause friction or stress on the bursa before it is healed will likely cause bursitis symptoms to flare up again.
Prevention
Because many soft tissue conditions are caused by overuse, the best treatment is prevention. It is important to avoid or modify the activities that cause problems. Underlying conditions such as leg length differences, improper position or poor technique in sports or work must be corrected. Be aware of potential overuse or injury in your daily activities and change your lifestyle to prevent problems. Otherwise, problems may persist or occur repeatedly. Following are some ways you can avoid future problems. Wear walking or jogging shoes that provide good support. High-top shoes provide support for people with ankle problems. Wear comfortable shoes that fit properly. Wear heel cups or other shoe inserts as recommended by your doctor. Exercise on level, graded surfaces.
Hammer Toe Ancestral Causes
There are two different types. Flexible Hammer toe. These are less serious because they can be diagnosed and treated while still in the developmental stage. They are called flexible hammertoes because they are still moveable at the joint. Rigid Hammertoes. This variety is more developed and more serious than the flexible condition. Rigid hammertoes can be seen in patients with severe arthritis, for example, or in patients who wait too long to seek professional treatment. The tendons in a rigid hammertoe have become tight, and the joint misaligned and immobile, making surgery the usual course of treatment.
Causes
A hammer toe develops because of an abnormal balance of the muscles in the toes. This abnormal balance causes increased pressures on the tendons and joints of the toe, leading to its contracture. Heredity and trauma can also lead to the formation of a hammer toe. Arthritis is another factor, because the balance around the toe in people with arthritis is disrupted. Wearing shoes that are too tight and cause the toes to squeeze can also cause a hammer toe to form.
.jpg%3Fformat%3D1500w) Symptoms
Symptoms
Hammer toe is often distinguished by a toe stuck in an upside-down ?V? position, and common symptoms include corns on the top of your toe joint. Pain at the top of a bent toe when you put on hammertoes your shoes. Pain when moving a toe joint. Pain on the ball of your foot under the bent toe. Corns developing on the top of the toe joint. It is advisable to seek medical advice if your feet hurt on a regular basis. It is imperative to act fast and seek the care of a podiatrist or foot surgeon. By acting quickly, you can prevent your problem from getting worse.
Diagnosis
The treatment options vary with the type and severity of each hammer toe, although identifying the deformity early in its development is important to avoid surgery. Your podiatric physician will examine and X-ray the affected area and recommend a treatment plan specific to your condition.
Non Surgical Treatment
Orthotics are shoe inserts that can help correct mechanical foot-motion problems to correct pressure on your toe or toes and reduce pain. Changing shoes. You should seek out shoes that conform to the shape of your feet as much as possible and provide plenty of room in the toe box, ensuring that your toes are not pinched or squeezed. You should make sure that, while standing, there is a half inch of space for your longest toe at the end of each shoe. Make sure the ball of your foot fits comfortably in the widest part of the shoe. Feet normally swell during the course of the day, so shop for shoes at the end of the day, when your feet are at their largest. Don't be vain about your shoe size, sizes vary by brand, so concentrate on making certain your shoes are comfortable. Remember that your two feet are very likely to be different sizes and fit your shoe size to the larger foot. Low-heel shoes. High heels shift all your body weight onto your toes, tremendously increasing the pressure on them and the joints associated with them. Instead, wear shoes with low (less than two inches) or flat heels that fit your foot comfortably.
Surgical Treatment
In some cases, usually when the hammertoe has become more rigid and painful, or when an open sore has developed, surgery is needed. Often patients with hammertoe have bunions or other foot deformities corrected at the same time. In selecting the procedure or combination of procedures for your particular case, the foot and ankle surgeon will take into consideration the extent of your deformity, the number of toes involved, your age, your activity level, and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
Hallux Valgus Surgery Aftercare
Overview
 A bunion is a bony enlargement of the joint and surrounding soft tissues at the base of the big toe. The enlargement makes the big toe joint stick out further on the side, and forces the big toe to curve in closer to the other toes. For some people, bunions cause little or no pain. In Canada, women are 10 times more likely than men to have bunions. Managing the condition so that it doesn't get worse is a matter of wearing appropriate footwear, cushioning and supporting the area, and taking pain relievers as required. People with more severe bunions may need more specific treatment, such as surgery.
A bunion is a bony enlargement of the joint and surrounding soft tissues at the base of the big toe. The enlargement makes the big toe joint stick out further on the side, and forces the big toe to curve in closer to the other toes. For some people, bunions cause little or no pain. In Canada, women are 10 times more likely than men to have bunions. Managing the condition so that it doesn't get worse is a matter of wearing appropriate footwear, cushioning and supporting the area, and taking pain relievers as required. People with more severe bunions may need more specific treatment, such as surgery.
Causes
Women traditionally have a higher rate of bunions, which is to be expected, since it is they who have traditionally worn shoes with high heels, a narrow toe box, or whatever fashion dictates from year to year. However, men can suffer from bunions as well, as can anyone for whom the right (or wrong) conditions exist, poor foot mechanics, improper footwear, occupational hazards, health and genetic predisposition. Finally, bunions have long been a condition associated with the elderly, and although they often appear in conjunction with inflammatory joint diseases such as arthritis (which is often associated with age), they can strike at any point in life, including adolescence.
Symptoms
Signs and symptoms of a bunion include the base of the big toe is swollen and sticks out. The big toe is often bent towards the other toes, and sometimes the second toe is pushed to overlap the third toe. Skin around the big toe joint is red and sore. Thickened skin at the base of the big toe. Pain in the big toe or foot. Wearing shoes is painful. Pain or difficulty when walking.
Diagnosis
Clinical findings are usually specific. Acute circumferential intense pain, warmth, swelling, and redness suggest gouty arthritis (see Gout) or infectious arthritis (see Acute Infectious Arthritis), sometimes mandating examination of synovial fluid. If multiple joints are affected, gout or another systemic rheumatic disease should be considered. If clinical diagnosis of osteoarthritic synovitis is equivocal, x-rays are taken. Suggestive findings include joint space narrowing and bony spurs extending from the metatarsal head or sometimes from the base of the proximal phalanx. Periarticular erosions (Martel sign) seen on imaging studies suggest gout.
Non Surgical Treatment
Padding with a number of different materials (eg felt) to reduce pressure on the painful prominence of the bunion. Physical therapy can be used to help with the symptoms and improve the range of motion (this is particularly helpful if the pain is coming from inside the joint, rather than from shoe pressure). Manipulation of the joint can be used to help with this (manipulation will never correct the alignment of the joint). Any corns and calluses that are causing symptoms should be treated. The correct fitting of footwear is essential for anyone who is serious about doing something about their bunions and hallux valgus. It may be possible to have your shoes stretched over the area of the bunion to also relieve pressure. Foot orthotics may be useful in helping with the instability about the joint. They may be more helpful if there are other symptoms in the foot as well, as their use in "treating" bunions is controversial. They may play a role in slowing progression and in the prevention of bunions developing again after surgical correction. Exercises can be important in maintaining the mobility of the joint in those with bunions, this is especially important for the arthritic type pains that may be originating from inside the joint and for the prevention of these painful symptoms in the future. 
Surgical Treatment
Surgery for bunions usually isn't done unless you have already tried other treatment and it did not relieve your pain. Other treatment includes wearing shoes with lots of room for your toes and using pads and supports in your shoe for protection and comfort. Surgery may be right for you if your toe is too painful, if your bunion is very big, or if you can't easily do your daily activities. It's not clear how well bunion surgery works or which kind of surgery is best. How well the surgery works depends on how bad your bunion is, the type of surgery you have, and your surgeon's experience. Your expectations will play a big role in how you feel about the results of surgery. If you want surgery mainly to improve the way your foot looks, you may be disappointed.
Overpronation Of The Feet
Over pronation of the foot is commonly referred to as "flat feet." Many middle-aged men and women suffer from over pronation over time and as a result of wearing poor-fitting shoes, continuing with repetitive exercising habits, or walking in high heels for long periods over several years. Regular speed-walkers often experience over pronation as well as a result of this activity.

Causes
Acquired "Flat Feet" this develops over a period of time rather than at birth (unlike Congenital "Flat Feet"). In children, many different factors may contribute to the development of this condition such as the type of shoes that a child wears, a child's sitting or sleeping positions or it may occur as some type of compensation for other abnormalities located further up the leg. Compensation may occur due to the rupture (tearing) of ligaments or tendons in the foot. One common reason for this condition is that the foot is compensating for a tight Achilles Tendon. If this tendon is tight it may cause the foot to point downward away from the body. This gives the body the perception that the affected leg is longer in length and the body attempts to compensate for the perceived additional length by flattening out the foot arch in an attempt to provide balance and stability.
Symptoms
Common conditions seen with overpronation include heel pain or plantar fasciitis. Achilles tendonopathy. Hallus Valgus and/or bunions. Patellofemoral pain syndrome. Iliotibial band pain syndrome. Low back pain. Shin splints. Stress fractures in the foot or lower leg.
Diagnosis
So, how can you tell if you have overpronation, or abnormal motion in your feet, and what plantar fasciitis treatment will work to correct it? Look at your feet. While standing, do you clearly see the arch on the inside of your foot? If not, and if the innermost part of your sole touches the floor, then your feet are overpronated. Look at your (running/walking) shoes. If your shoes are more worn on the inside of the sole in particular, then pronation may be a problem for you. Use the wet foot test. Wet your feet and walk along a section of pavement, then look at the footprints you leave behind. A normal foot will leave a print of the heel connected to the forefoot by a strip approximately half the width of the foot on the outside of the sole. If you?re feet are pronated there may be little distinction between the rear and forefoot.
Non Surgical Treatment
Overpronation is a condition in which the foot rolls excessively down and inward. The arch may elongate and collapse (or ?fall?) and the heel will lean inward. Overpronation should not be confused with pronation. Pronation is a normal motion of the foot during weight bearing and allows the foot to absorb shock as it contacts the ground.
Prevention
Many of the prevention methods for overpronation orthotics, for example, can be used interchangeably with treatment methods. If the overpronation is severe, you should seek medical attention from a podiatrist who can cast you for custom-made orthotics. Custom-made orthotics are more expensive, but they last longer and provide support, stability, and balance for the entire foot. You can also talk with a shoe specialist about running shoes that offer extra medial support and firm heel counters. Proper shoes can improve symptoms quickly and prevent them from recurring. Surgery can sometimes help cure and prevent this problem if you suffer from inherited or acquired pes planus deformity. Surgery typically involves stabilizing the bones to improve the foot?s support and function.
Will Calcaneal Apophysitis Often Require Surgical Treatments?
What is sever's disease? sever's disease is a common cause of heel pain in active children. Sever's disease, also called calcaneal apophysitis, occurs when the growth plate of the heel is injured by excessive forces during early adolescence.
Causes
During the growth spurt of early puberty, the heel bone (also called the calcaneus) sometimes grows faster than the leg muscles and tendons. This can cause the muscles and tendons to become very tight and overstretched, making the heel less flexible and putting pressure on the growth plate. The Achilles tendon (also called the heel cord) is the strongest tendon that attaches to the growth plate in the heel. Over time, repeated stress (force or pressure) on the already tight Achilles tendon damages the growth plate, causing the swelling, tenderness, and pain of Sever's disease. Such stress commonly results from physical activities and sports that involve running and jumping, especially those that take place on hard surfaces, such as track, basketball, soccer, and gymnastics.
Symptoms
Acute pain, pain asscoiatied with Sever?s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running. Highly active - children who are very active are among the most susceptible in experiencing Sever?s disease, because of the stress and tension placed on their feet.
Diagnosis
You may have pain when your doctor squeezes your heel bone. You may have pain when asked to stand or walk on your toes or on your heels. You may have pain in your heel when your doctor stretches your calf muscles. Your doctor may order x-rays of the injured foot to show an active growth plate.
Non Surgical Treatment
Reduce inflammation:
Ice: For at least 20 minutes after activity or when pain increases.
Nonsteroidal anti-inflammatory drugs:(NSAIDs) may also help. Stretch the calf. Increase calf flexibility by doing calf stretches for 30 to 45 seconds several times per day.
Protect the heel: The shoe may need to be modified to provide the proper heel lift or arch support.
Select a shoe with good arch support and heel lift if possible. Try heel lifts or heel cups in sports shoes, especially cleats. Try arch support in cleats if flat feet contribute to the problem.
Take it one step at a time:. Gradually resume running and impact activities as symptoms allow. Sever?s disease usually goes away when the growth plate (apophysis) matures, which should be by age 12 to 13 years in females and 13 to 14 years in males.
Surgical Treatment
The surgeon may select one or more of the following options to treat calcaneal apophysitis. Reduce activity. The child needs to reduce or stop any activity that causes pain. Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue. Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile. Often heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis, or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.
Acquired Flat Foot Tibialis Posterior Tenosynovitis
Overview
The posterior tibial tendon serves as one of the major supporting structures of the foot, helping it to function while walking. Posterior tibial tendon dysfunction (PTTD) is a condition caused by changes in the tendon, impairing its ability to support the arch. This results in flattening of the foot. PTTD is often called ?adult acquired flatfoot? because it is the most common type of flatfoot developed during adulthood. Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse, especially if it isn?t treated early. 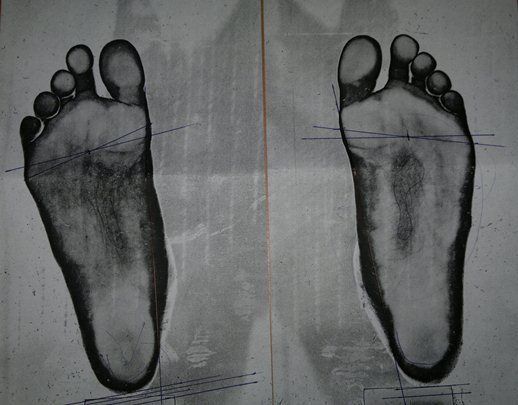
Causes
As discussed above, many different problems can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to support the arch of your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Inflammatory arthritis, such as rheumatoid arthritis, can cause a painful flatfoot. This type of arthritis attacks not only the cartilage in the joints, but also the ligaments that support the foot. Inflammatory arthritis not only causes pain, but also causes the foot to change shape and become flat. The arthritis can affect the back of the foot or the middle of foot, both of which can result in a fallen arch. An injury to the tendons or ligaments in the foot can cause the joints to fall out of alignment. The ligaments support the bones and prevent them from moving. If the ligaments are torn, the foot will become flat and painful. This more commonly occurs in the middle of the foot (Lisfranc injury), but can also occur in the back of the foot. Injuries to tendons of the foot can occur either in one instance (traumatically) or with repeated use over time (overuse injury). Regardless of the cause, if tendon function is altered, the forces that are transmitted across joints in the foot are changed and this can lead to increased stress on joint cartilage and ligaments. In addition to tendon and ligament injuries, fractures and dislocations of the bones in the midfoot can also lead to a flatfoot deformity. People with diabetes or with nerve problems that limits normal feeling in the feet, can have collapse of the arch or of the entire foot. This type of arch collapse is typically more severe than that seen in patients with normal feeling in their feet. In addition to the ligaments not holding the bones in place, the bones themselves can sometimes fracture and disintegrate without the patient feeling any pain. This may result in a severely deformed foot that is very challenging to correct with surgery. Special shoes or braces are the best method for dealing with this problem.
Symptoms
Many patients with this condition have no pain or symptoms. When problems do arise, the good news is that acquired flatfoot treatment is often very effective. Initially, it will be important to rest and avoid activities that worsen the pain.
Diagnosis
In the early stages of dysfunction of the posterior tibial tendon, most of the discomfort is located medially along the course of the tendon and the patient reports fatigue and aching on the plantar-medial aspect of the foot and ankle. Swelling is common if the dysfunction is associated with tenosynovitis. As dysfunction of the tendon progresses, maximum pain occurs laterally in the sinus tarsi because of impingement of the fibula against the calcaneus. With increasing deformity, patients report that the shape of the foot changes and that it becomes increasingly difficult to wear shoes. Many patients no longer report pain in the medial part of the foot and ankle after a complete rupture of the posterior tibial tendon has occurred; instead, the pain is located laterally. If a fixed deformity has not occurred, the patient may report that standing or walking with the hindfoot slightly inverted alleviates the lateral impingement and relieves the pain in the lateral part of the foot.
Non surgical Treatment
Non-surgical treatment includes rest and reducing your activity until the pain improves. Orthotics or bracing help support the tendon to reduce its pull along the arch, thus reducing pain. In moderate to severe cases, a below knee cast or walking boot may be needed to allow the tendon to rest completely and heal. Physical therapy is an integral part of the non-surgical treatment regimen to reduce inflammation and pain. Anti-inflammatory medication is often used as well. Many times evaluation of your current shoes is necessary to ensure you are wearing appropriate shoe gear to prevent re-injury. 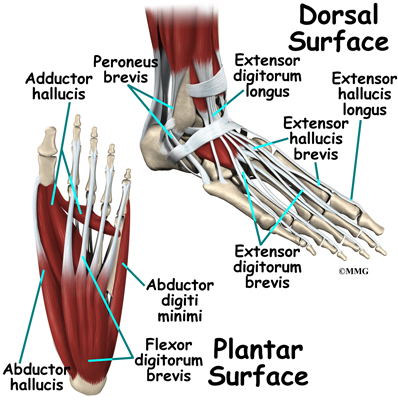
Surgical Treatment
Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
What Is The Treatment And Cause For Adult Aquired FlatFoot
One in four adults in the U.S. has adult acquired flatfoot deformity, which may begin during childhood or be acquired with age. The foot may be flat all the time or may lose its arch when the person stands. The most common and serious cause of flat foot is Posterior Tibial Tendon Dysfunction, in which the main tendon that supports the arch gradually weakens.

Causes
There are numerous causes of acquired Adult Flatfoot, including, trauma, fracture, dislocation, tendon rupture/partial rupture or inflammation of the tendons, tarsal coalition, arthritis, neuroarthropathy and neurologic weakness. The most common cause of acquired Adult Flatfoot is due to overuse of a tendon on the inside of the ankle called the posterior tibial tendon. This is classed as - posterior tibial tendon dysfunction. What are the causes of Adult Acquired flat foot? Trauma, Fracture or dislocation. Tendon rupture, partial tear or inflammation. Tarsal Coalition. Arthritis. Neuroarthropathy. Neurological weakness.
Symptoms
Often, this condition is only present in one foot, but it can affect both. Adult acquired flatfoot symptoms vary, but can swelling of the foot's inner side and aching heel and arch pain. Some patients experience no pain, but others may experience severe pain. Symptoms may increase during long periods of standing, resulting in fatigue. Symptoms may change over time as the condition worsens. The pain may move to the foot's outer side, and some patients may develop arthritis in the ankle and foot.
Diagnosis
There are four stages of adult-acquired flatfoot deformity (AAFD). The severity of the deformity determines your stage. For example, Stage I means there is a flatfoot position but without deformity. Pain and swelling from tendinitis is common in this stage. Stage II there is a change in the foot alignment. This means a deformity is starting to develop. The physician can still move the bones back into place manually (passively). Stage III adult-acquired flatfoot deformity (AAFD) tells us there is a fixed deformity. This means the ankle is stiff or rigid and doesn???t move beyond a neutral (midline) position. Stage IV is characterized by deformity in the foot and the ankle. The deformity may be flexible or fixed. The joints often show signs of degenerative joint disease (arthritis).
Non surgical Treatment
Medical or nonoperative therapy for posterior tibial tendon dysfunction involves rest, immobilization, nonsteroidal anti-inflammatory medication, physical therapy, orthotics, and bracing. This treatment is especially attractive for patients who are elderly, who place low demands on the tendon, and who may have underlying medical problems that preclude operative intervention. During stage 1 posterior tibial tendon dysfunction, pain, rather than deformity, predominates. Cast immobilization is indicated for acute tenosynovitis of the posterior tibial tendon or for patients whose main presenting feature is chronic pain along the tendon sheath. A well-molded short leg walking cast or removable cast boot should be used for 6-8 weeks. Weight bearing is permitted if the patient is able to ambulate without pain. If improvement is noted, the patient then may be placed in custom full-length semirigid orthotics. The patient may then be referred to physical therapy for stretching of the Achilles tendon and strengthening of the posterior tibial tendon. Steroid injection into the posterior tibial tendon sheath is not recommended due to the possibility of causing a tendon rupture. In stage 2 dysfunction, a painful flexible deformity develops, and more control of hindfoot motion is required. In these cases, a rigid University of California at Berkley (UCBL) orthosis or short articulated ankle-foot orthosis (AFO) is indicated. Once a rigid flatfoot deformity develops, as in stage 3 or 4, bracing is extended above the ankle with a molded AFO, double upright brace, or patellar-tendon-bearing brace. The goals of this treatment are to accommodate the deformity, prevent or slow further collapse, and improve walking ability by transferring load to the proximal leg away from the collapsed medial midfoot and heel.

Surgical Treatment
If conservative treatment fails to provide relief of pain and disability then surgery is considered. Numerous factors determine whether a patient is a surgical candidate. They include age, obesity, diabetes, vascular status, and the ability to be compliant with post-operative care. Surgery usually requires a prolonged period of nonweightbearing immobilization. Total recovery ranges from 3 months to one year. Clinical, x-ray, and MRI examination are all used to select the appropriate surgical procedure.